Front Oncol:局部晚期鼻咽癌三种诱导化疗的疗效和毒性:10年随访结果
时间:2021-10-14 21:01:22 热度:37.1℃ 作者:网络
目前局部晚期鼻咽癌患者通常在同步放化疗前(CRT)使用诱导化疗(IC)。IC的应用可改善患者的无远处转移生存期(DMFS)和总生存期(OS)。一项回顾性研究发现多西他赛+顺铂+5-FU(TPF)比多西他赛+顺铂(TP)或顺铂+ 5-氟尿嘧啶(PF)的效果更好。但是,不足的是随访时间不足,且有些患者并没有后续同步放化疗。因此,来自中山大学肿瘤医院的团队开展了回顾性研究,旨在比较多西紫杉醇+顺铂+5-FU(TPF)、多西紫杉醇+顺铂(TP)和顺铂+ 5-FU(PF)联合同步放化疗(CRT)治疗局部晚期鼻咽癌(NPC)的10年生存率。相关结果发表在Frontiers in Oncology杂志上。
纳入主要纳入符合条件的新诊断III-IVA期鼻咽癌患者。倾向评分匹配(PSM)用于平衡预后协变量。比较各组的生存情况和毒性。
2009年4月至2012年12月共纳入855例患者,其中395例(46.2%)接受TPF + CRT治疗,258例(30.2%)接受TP + CRT治疗,202例(23.6%)接受PF + CRT治疗。总体人群的平均年龄为44岁。与TPF + CRT和TP + CRT组相比,PF + CRT组T4 (29.4% vs. 39.3% vs. 35.2%, P = 0.007)、N3 (14.7% vs. 20.7% vs. 23.3%, P = 0.173)和IVA期(41.1% vs. 55.7% vs. 52.0%, P = 0.001)的比例较低。与TP + CRT和PF + CRT组相比,TPF + CRT组接受3个或3个以上周期的患者更多(69.6% vs. 22.3% vs. 26.7%, P<0.0001)。值得注意的是,TP + CRT组接受顺铂累计剂量(CCD) ≥200 mg/ m2的患者比例最低(8.9% vs. 23.0% vs. 21.7%,P<0.0001)。
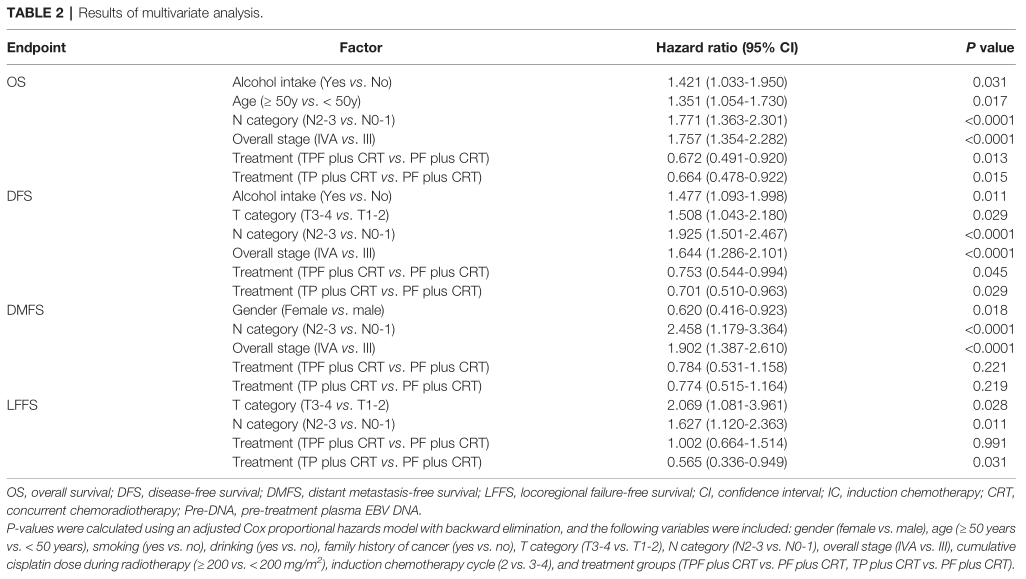
总体人群10年OS、DFS(无病生存期)、DMFS和LFFS(无局部治疗失败生存)率分别为67.8%, 64.9%, 78.4%和83.8%。对于OS,TPF vs TP vs PF组的10年生存率为67.7% vs 73.5% vs 60.5% (P TPF vs. TP = 0.153, P TPF vs. PF = 0.058, P PF vs. TP = 0.003);对于DFS,TPF vs TP vs PF组为63.6% vs. 71.1% vs. 59.2% (P TPF vs. TP = 0.055, P TPF vs. PF = 0.262, P PF vs. TP = 0.007);对于DMFS,TPF vs TP vs PF组为77.7% vs. 82.3% vs. 74.5% (P TPF vs. TP = 0.209, P TPF vs. PF = 0.39, P PF vs. TP = 0.063);对于LFFS,TPF vs TP vs PF组为81.2% vs. 89.5% vs. 81.8% (P TPF vs. TP = 0.006, P TPF vs. PF = 0.968, P PF vs. TP = 0.015)。通过调整Cox比例风险模型调整各种因素后,与PF + CRT相比,TPF + CRT (OS: HR, 0.672;95%CI, 0.491 0.920;P = 0.013; DFS:HR,0.753;95% CI, 0.544 0.994;P = 0.045)和TP + CRT (OS: HR, 0.664;95%CI, 0.478 0.922;P = 0.015;DFS:HR,0.701;95%CI, 0.510 0.963;P = 0.029)显著改善患者的OS和DFS。
预后相关因素
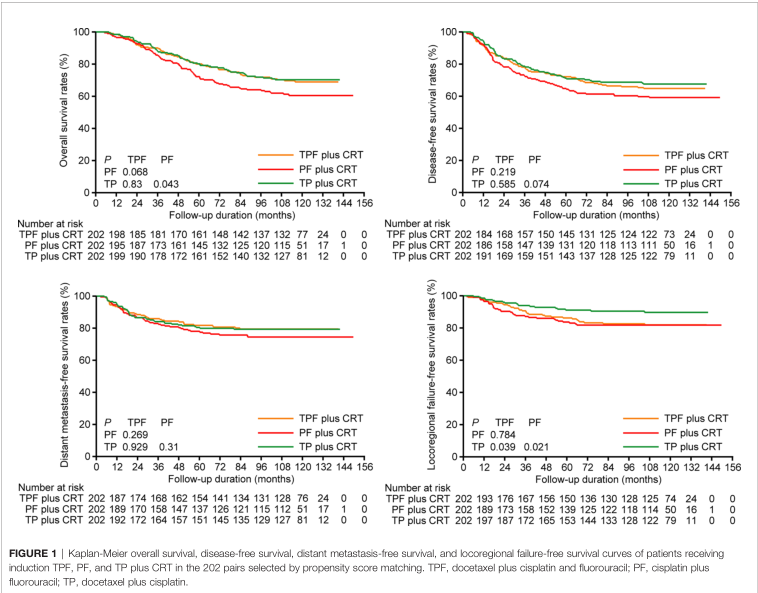
经过PSM匹配后,TPF vs. PF vs. TP组的10年 OS, DFS, DMFS, 以及LFFS率分别为 68.9% vs.70.3% vs. 60.5% (P TPF vs. TP = 0.83, P TPF vs. PF = 0.068, P PF vs. TP = 0.043), 64.8% vs. 67.6% vs. 59.2% (P TPF vs. TP = 0.585, P TPF vs. PF =0.219, P PF vs. TP = 0.074), 79.5% vs. 79.3% vs. 74.5% (P TPF vs. TP =0.929, P TPF vs. PF = 0.269, P PF vs. TP = 0.310), 以及81.9% vs. 89.7%vs. 81.8% (P TPF vs. TP = 0.039, P TPF vs. PF = 0.784, P PF vs. TP = 0.021)。多因素分析结果显示,与PF + CRT比较,TPF + CRT (HR, 0.617; 95%CI, 0.426 - -0.894;P = 0.011), TP + CRT (HR, 0.699; 95%CI,0.498-0.982;P = 0.039)显著改善了OS,但DFS 不明显(TPF + CRT: HR, 0.701;95%CI, 0.491 - 1.002;P = 0.051;TP + CRT: HR, 0.738;95%CI, 0.532 - 1.025;P = 0.07)。
PSM后预后分析
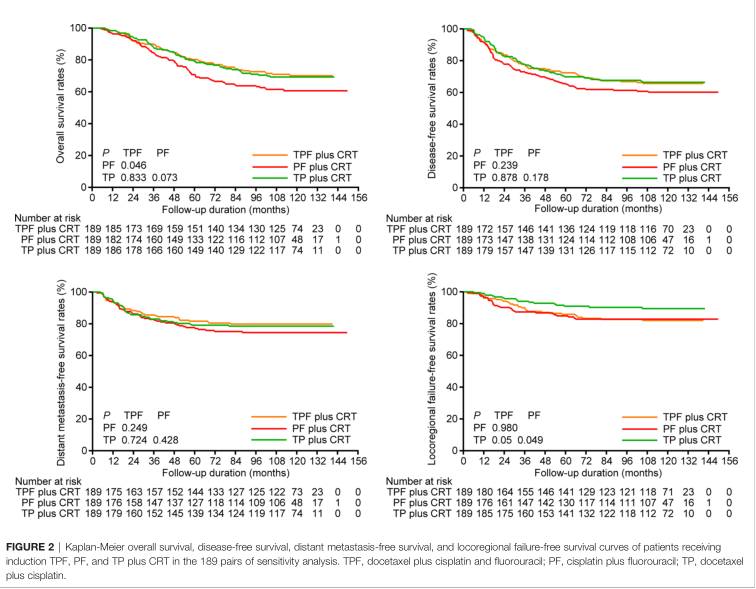
敏感性分析发现,与上述结果一致,TPF + CRT和TP + CRT仍然比PF + CRT获得了更高的10年OS (70.1% vs. 69.3% vs. 60.6%)、DFS (65.7% vs. 66.4% vs. 60.2%)和DMFS (79.8% vs. 78.5% vs. 74.4%)率。
敏感分析预后
跟预期一样,PF方案的3-5级毒性发生率最低(27.3%),TP方案的3-5级毒性发生率最高,主要为3-5级中性粒细胞减少(97.1%)和发热性中性粒细胞减少(11.8%)。此外,TP组3 - 5级非血液学毒性不常见。与PF方案相比,TPF方案出现较高的3 ~ 5级中性粒细胞减少(35.6% vs. 14.7%, P<0.001),白细胞减少(27.2% vs. 5%, P<0.001)和粘膜炎(6.3% vs. 1.3%, P = 0.004)。毫无疑问,多西他赛加到PF中会导致更大的毒性。
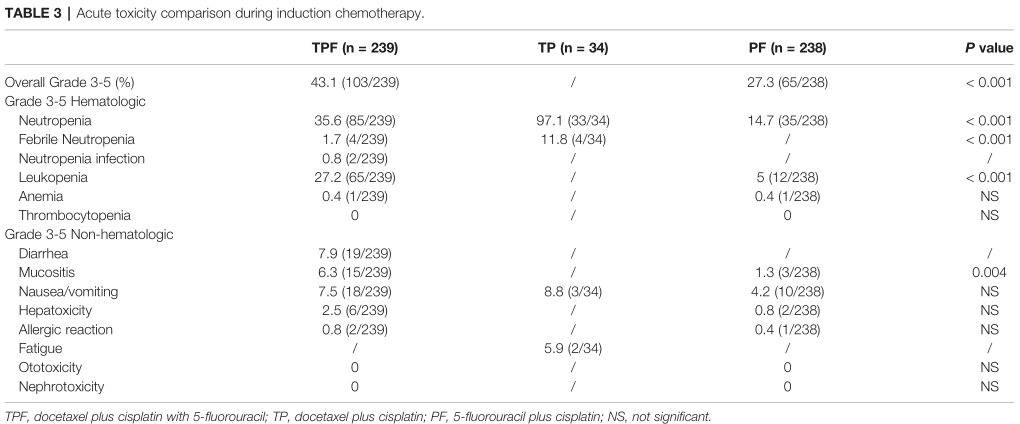
不良反应对比
综上,研究表明,对于III-IVA期NPC患者,TPF+CRT 和TP+ CRT较PF+CRT改善患者的10年OS。
原始出处:
Peng H, Chen B, He S, Tian L and Huang Y (2021) Efficacy and Toxicity of Three Induction Chemotherapy Regimens in Locoregionally Advanced Nasopharyngeal Carcinoma: Outcomes of 10-Year Follow-Up. Front. Oncol. 11:765378. doi: 10.3389/fonc.2021.765378


